If you have difficulty accessing this page, which gives a round-up of FPH’s activities in 2015, please email policy@fph.org.uk for a plain text version of it.


Posted in Uncategorized on December 18, 2015| Leave a Comment »
If you have difficulty accessing this page, which gives a round-up of FPH’s activities in 2015, please email policy@fph.org.uk for a plain text version of it.


Posted in Uncategorized on December 14, 2015| Leave a Comment »
The second meeting of the Faculty of Public Health’s Strategic Interest Group for Sustainable Development on 4 December began with a reminder of the reasons why it is important for us to tackle climate change.
This was clearly illustrated by the photograph below of Cockermouth’s public illustration of the height of their floods in 2009. Following the flooding, new and improved flood defences were installed.
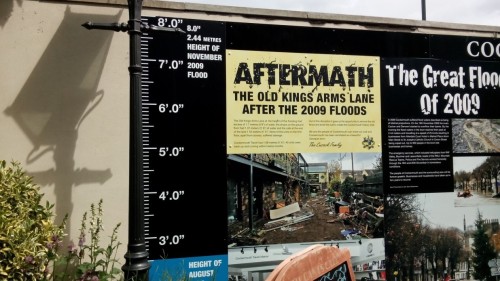
Cockermouth’s public illustration of the height of their floods in 2009
However, they did not protect homes and businesses in the area from the severe weather event that occurred during the first week of December 2015 in the Lake District. Our thoughts go out to all those who have suffered as a result of the flooding, many of whom have experienced this for the second or third time in 10 years.
Evidence from the Lancet Commission and the Intergovernmental Panel on Climate Change (IPCC) confirms that an unsustainable approach to the future (including climate change) is almost certainly one of the biggest threats to public health this century. Tackling this needs a transformation in the way our industries (including the health sector) and we as individuals carry out our business and day-to-day lives. The evidence is clear and widely accepted that inaction is unacceptable; the multiple benefits for health are profound; and time is running out.
We were joined at this meeting by:
They offered their insights into Public Health and Sustainable Development in a Local Authority setting and Fernando Antezana-Aranibar: former Deputy Director General of the World Health Organisation gave his international perspective about Climate Change and health.
Key points emerging included:
Progress
• The FPH is one of the leading UK organisations to publish on health, sustainable development and climate change.
• There is already a significant reference to climate change and sustainable development manifesto in the most recent manifesto from the FPH.
• A well consulted national cross system strategy exists for the entire health and care system which is closely aligned with the values and remit of FPH members.
• There is a clear commitment from the FPH on Environmental Sustainability & Public Health Training in the UK with placements available in organisations such as the Sustainable Development Unit. • The new Public Health Training Curriculum (2015) recognises that sustainability is fundamental and cuts across the entire curriculum; and includes a new learning outcome, “Demonstrate leadership in environmental sustainability with a focus on the links to health and climate change”.
• And finally, FPH has close links with the Climate and Health Council and is a founder member of the Alliance of the newly formed Health Professionals Alliance for Combating Climate Change (HACC) 2015.
The new FPH SIG is now developing a strategic work plan that takes a whole system approach which addresses human activity and health in its social, environmental, economic and cultural complexity coordinate action and provide leadership and strong voice – to support the organisation internally and its members, fellows and partners more widely.
The time is right to seize the day, build on FPH’s work on Sustainable Development and assure the future.
With thanks to David Pencheon, Lindsey Stewart, Femi Biyibi, James Smith, Jane Beenstock, Jilla Burgess, Sue Atkinson and Simon Capewell and all participants for their contributions and encouragement.
Posted in Climate change, Global Health, Uncategorized, tagged Climate change, UN climate change conference on December 10, 2015| Leave a Comment »
I am in Paris – for COP 21.
COP 21 (21st Conference of the Parties) of the UN Framework on Climate Change (UNFCCC) are the negotiations between the 195 countries attending, to make a deal to curb emissions and keep global warming below 2°C.
I am not at the main COP negotiations in Le Bourget but at the Global Climate and Health Alliance (GCHA) Health Summit and other parallel health meetings.
Unfortunately the timing of the Summit means I missed the FPH ‘Sustainable development and health’ SIG meeting in Nottingham on 4th December which followed the instigation of the SIG at the Faculty Conference in June.
People are starting to recognise the importance of health, climate change and sustainability and accepting what the Lancet commission identified in 2009, that ‘Climate Change (CC) could be the biggest global threat of the 21st Century’.
The Health Summit was the buzziest conference in ages. Over 500 people and oversubscribed, it was chaired (amusingly and with clear insights) by John Vidal (Environment Editor for the Guardian) and attendees included Health Ministers, the Deputy Mayor of Paris, WHO and GIZ (Deutsche Gesellschaft für Internationale Zusammenarbeit, the German equivalent of DFID), who both supported the conference (thank you), representatives of health and climate change groups and alliances from across the globe.
The presentations, parallel sessions and panel discussions were informative, interesting, lively, amusing, challenging and enjoyable with many interesting discussions taking place around the edges with an exchange of shared ideas and experiences to take back home.
Some of the snippets I picked up included:
And much much more …
We have come a long way since COP15 in Copenhagen in 2009, when those of us interested in health and climate change could fit around one small coffee table and it now feels as though the importance of health in the climate change negotiations is starting to make its mark.
CC science is real but it is often difficult to get our heads round and some of the environmental and other impacts seem like a long way off and we know that politicians and all of us (including teenagers) find it hard to recognise and take action on threats that are in the more distant future.
Health brings home the real story of the impact of climate change – imperative, immediate and life changing.
Families displaced because of floods and typhoons, children starving as a result of drought resulting in failing crops, older people dying in heat-waves, even as recently and as nearby as 15,000 deaths in France in 2003.
With 500 people still dying annually of Malaria, the 2.5 million people suffering from the disease could increase again to over four million with the spread of mosquitos due to climate change.People are sick and dying from lack of clean water as a result of either drought or destruction of infrastructure by severe storms and tsunamis.
Closer to home, just this weekend the floods in Cumbria have caused distress and destruction as well as the financial costs of these storms. And of course the important links between climate change, disasters and water shortages, refugees and terrorism.

Recent floods in the north of England (like York City Centre, pictured) have brought home the reality of climate change to the UK
The latest Lancet Commission (2015) identified that ‘Tackling CC could be the greatest health opportunity of the 21st century’.
The health summit felt both daunting and optimistic. We must act now.
The spoken word poet – Sophia Walker – captured it in her piece written for the Health Summit as “…we aren’t just talking about the weather” and suggested that nine billion people on the planet could work ‘miracles’ if they all did their bit.
We in public health must do ours, not just individually but in whatever ways we can through our building it into our daily work, e.g. identifying the co-benefits of improving health and the environment. It seems that at last the penny may be dropping that climate change and health are inexplicably linked. What’s good for health is good for the planet.
References
Lancet Commission. 2009. “Managing the health effects of climate change”. Lancet and UCL Institute for Global Health Commission. April 2009.
Lancet Commission.2015. “Health and Climate Change: policy responses to protect public health” Lancet. June 2015.
Posted in Uncategorized on December 7, 2015| Leave a Comment »
To ‘save money’ to boost struggling health services the Chancellor has decided to cut funding for public health and prevention, reducing spending on public health as a proportion of all health expenditure from 3.5% in 2015 to 2.5% by 2020.
The government has reneged on its 2010 commitment to “re-balance the focus on the causes of ill health and ensure that public health funding is prioritised”. The flawed logic of cutting investment in cost saving preventative services, such as sexual health, family planning, smoking cessation, drug, alcohol and child health services is strikingly short sighted.
But what is even more worrying is that these cuts are likely to be greatest in the poorest areas with the greatest need, reversing progress that has been made to address health inequalities. From the late 1990s a systematic strategy was implemented in England to reduce differences in health between the most deprived parts of the country and more affluent areas.
One consequence of this strategy was to prioritise investment in public health in more deprived parts of the country, leading to levels of spending in these areas that are around two and a half times higher, per head of population, than in more affluent areas.
There is growing evidence that this strategy worked (1,2). Figure 1 shows decreasing absolute inequality in premature mortality between more affluent and more deprived local authorities (LAs) from the late 1990s onwards during the time of the health inequalities strategy. The strategy was associated with a reversal in the previous trend of increasing inequalities.

Figure 1: difference in under 75 year old mortality, between most deprived and most affluent 20% of LAs (Source: Office for National Statistics)
The chancellor’s spending review outlines an average real terms cut in the public health budget of 3.9% each year over the next 5 years. This translates into a cash reduction of 9.6% in addition to the £200 million cut that was announced earlier this year. The implications for individual LAs will depend on the way the funding formula is applied and the decision about “pace of change”.
The Department of Health is currently consulting on a new formula for the public health allocation. The application of this formula will reduce the share of resources going to more deprived areas relative to more affluent areas. This is because it allocates about twice the amount of resources per head to more deprived LAs compared to more affluent ones, whilst currently these areas receive about two and a half times the amount of resources per head.
There are a number of ways the Department of Health could distribute these cuts across LAs. They could apply a flat 9.6% cut to each LA over the next 5 years. This was the approach taken to allocating the cut of £200 million announced early this year, with each LA receiving a 6.2% cut. This approach will tend to widen inequalities, since the same percentage cut for an LA in a more deprived area, translates into a higher cut per head of population, compared to a more affluent LA. This is because more deprived LAs, with higher needs, have higher baseline funding than more affluent LAs.
But this approach would not involve using the new formula at all, and one might wonder what would be the point of having an allocation formula if its not going to be used. So a likely option would be to distribute the cuts so that those LAs most over target receive a higher cut than those most under target; over time moving all LAs towards their target allocation. Since, on average, more deprived LAs are more likely to be assessed as ‘over target’ according to the new formula, this will tend to lead to even higher cuts in more deprived areas compared to just applying a flat percentage cut to all LAs.
In fact, all of the likely scenarios will hit the poorest areas hardest. Figure 2 below shows the cuts each year from 2015 experienced by the most affluent and most deprived 20% of LAs under 4 scenarios, (1) applying a the same percentage cut to all LAs, (2) applying a higher cut to more “over target” LAs but setting the maximum cut in any year for any LA at 4%, (3) applying a higher cut to more “over target” LAs but setting the maximum cut in any year at 8%,(4) applying a higher cut to more “over target” LAs so that all LAs reach their target allocation by 2020.
Note that these scenarios do not take into account the government’s additional proposal to fully fund local authorities’ public health spending from business rates which could further reduce funding in the poorest areas.

Figure 2: planned cut in public health funds in most affluent and most deprived 20% of LAs under four potential scenarios for distributing the cuts (Sources: Local authority public health grant allocations 2015/16 – Spending Review and Autumn Statement 2015 – Duncan Selbie’s letter to LA CE)
The progress that has been made in recent years to reduce health inequalities shows that the level and distribution of public health resources makes a difference. Cutting public heath services in this manner makes no financial sense; it will harm the public’s health and will increase health inequalities.
1 Barr B, Bambra C, Whitehead M. The impact of NHS resource allocation policy on health inequalities in England 2001-11: longitudinal ecological study. BMJ 2014; 348: g3231–g3231.
2 Buck D, Maguire D. Inequalities in life expectancy – Changes over time and implications for policy. The Kings Fund, 2015 (accessed Nov 30, 2015).
Posted in Uncategorized on December 1, 2015| 1 Comment »
Worlds AIDS Day will be marked on 1st December 2015. Though HIV is no longer the deadly disease associated with the initial epidemic in the 1980s and 1990s, it remains an important public health issue today in the UK.
It is estimated that 103,700 people in the UK are living with HIV and around one fifth (17%) of these are thought to be unaware of their diagnosis. It is more common among men who have sex with men (MSM) and black African men and women. Geographically, high HIV prevalence is found in London and in pockets outside of the capita,l for example in Brighton and Hove and Manchester.
All but one of the London boroughs had a diagnosed HIV prevalence rate of above 2 per 1,000 in 2014. This is considered high and above the threshold for routine testing of new GP registrants, so HIV is a significant public health problem in London.
One of the key public health challenges is to improve the early diagnosis of HIV and thus prevent transmission and enable early treatment initiation. Late diagnosis of HIV is associated with higher mortality so ensuring that those at risk get tested is a priority. The number of people living with HIV continues to rise in the UK. With the introduction of effective anti-retroviral therapy, if detected early people living with HIV can expect a near normal life expectancy. However reducing the entrenched stigma associated the disease remains a challenge.
HIV prevention can be through a number of initiatives. Promoting consistent safe condom use is vital and needs to be focused particularly among key risk groups such as MSM.
Targeted and relevant safe sex messages are needed for MSM, particularly those likely to engage in HIV transmission risky behaviours such as having multiple casual partners, making assumptions about HIV status, and those who recreationally use drugs prior or during sexual intercourse: termed ‘chemsex’.
Increasing HIV testing rates is also a key prevention initiative to reduce onward transmission and new innovative ways to improve access and uptake of HIV testing are being developed.
There are many national and local initiatives aimed at improving HIV testing rates and promoting safe sex. For example National HIV Testing week runs in the week prior to Worlds AIDS day and promotes HIV testing nationally. This year saw the launch of the ‘National HIV Self-Testing Service’, funded by local authorities in conjunction with Public Health England.
In the capital, where almost half of all HIV cases are diagnosed, ‘Do it London’ is the campaigning element of the multi-faceted London HIV Prevention Programme (LHPP). This is a London-wide sexual health promotion initiative aimed at increasing HIV testing and promoting safer sex to all residents in the capital, funded by every London borough according to their diagnosed HIV prevalence.
As well as the city-wide Do It London campaign to promote HIV testing, the LHPP also provides free and low-cost condoms in over 80 London gay clubs, bars and saunas, supported by a highly specialised gay men’s outreach service which targets high risk men for health promotion interventions and on-the-spot rapid HIV testing.
In Lambeth and Southwark, which experience high levels of sexually transmitted infections and the highest HIV rates in England, SH:24 is leading the way in improving access to sexual health screening for residents by using internet and telephone technologies to deliver sexual health care remotely, 24 hours a day, seven days a week.
SH24 is fully integrated with local NHS services and enables Lambeth and Southwark residents who are concerned about their sexual health to log onto the SH24 website, receive health information, signposting to services and order a STI testing kit (including HIV) to be delivered to their home. They take a sample themselves at home, post it to the laboratory and receive results by text or from a local clinic depending on whether or not treatment is required. User feedback has been overwhelming positive and activity has continued to increase since the service went live in March 2015.
Looking to the future of HIV prevention and management, easier access to testing is vital to reduce the burden of disease caused by late diagnoses. Innovative solutions such as SH:24 will likely expand nationally and receive greater focus as these programs improve access to HIV testing whilst realising cost savings for local sexual health commissioners.
Many local authorities have signed up to the ‘Halve It’ initiative, including Lambeth and Southwark. This is a national coalition of experts brought together with the aim of tackling the public health challenges of HIV: namely halving the proportion of people diagnosed late with HIV and halving the proportion of people living with undiagnosed HIV by 2020. ‘Halve It’ is now also working with the London HIV Prevention Programme. Its shared aims should be recognised and endorsed by everyone working within public health in the UK.
Significant progress has been made over the last decade in the treatment of HIV. The challenge now is to ensure we work to achieve the aspirations set out in the Halve It campaign through a multi-faceted and targeted programme of increasing access to testing amongst high risk groups.
Key References